Introduction
In general, hyperplastic polyps are benign in nature and they do not have any malignant potential. However, right colonic hyperplastic polyps should be removed as well. Inflammatory polyps are usually not premalignant.
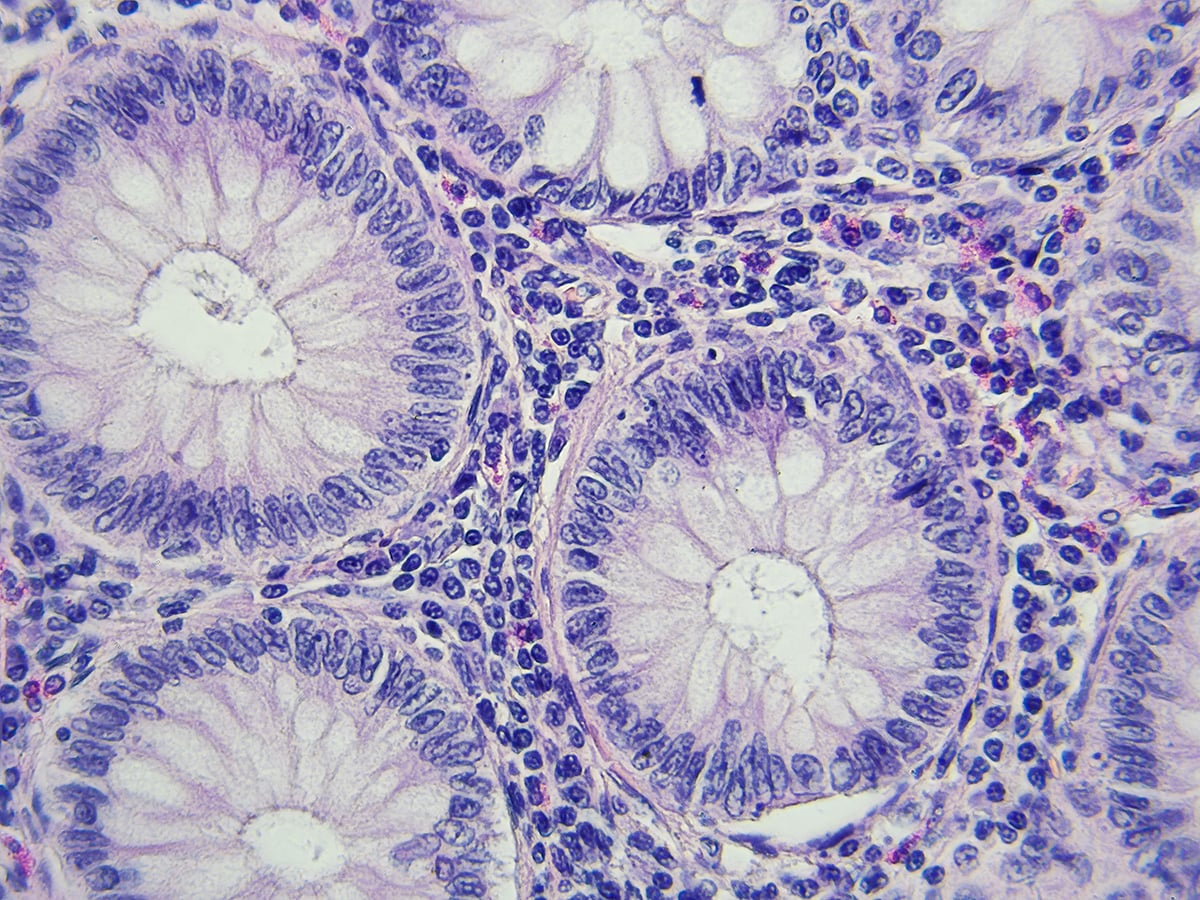
Adenomatous polyps are of three types: tubular adenomas, villous adenomas and tubulovillous adenomas.
- Tubular adenomas are the most common form of polyp, but it has the least chance of growing into malignancy.
- Villous adenomas are truly premalignant and they need definitely to be excised. Mucus discharge and hypokalaemia are more common with this type of polyp.
- Tubulovillous adenomas are another type of growth that could become cancerous, and these can grow within other areas of the body.
Polyps can become problematic if there are more villous elements in the formations. The shape of the growth also determines its potential for harm. For instance, flatter polyps are more worrisome than ones that have stalks. Flat polyps are dangerous because they contain shorter entryways for damaging cells, and they are harder to remove. When the cells change their shape and become abnormal, they become indeed premalignant. They are called Dysplastic cells
Risk Factors
These are: Type 2 diabetes, heavy alcohol use, a family history of colon cancer, hereditary nonpolyposis colon cancer, obesity, smoking, and a diet rich in processed and red meats. Colon cancer is most common in individuals who are over the age of 50.
Symptoms
- Adenomatous polyps have the potential to become cancerous.
- Rectal bleeding can be a sign of cancer or other conditions such as haemorrhoids or minor tears in the anus. In some patients, blood shows up as red streaks in the stool or makes the stool look black. The alteration of colour may also be because of foods, medications or supplements.
- Constipation or diarrhea that lasts for more than a week can be an indication of the presence of a large colon polyp. However, several other conditions can also cause a change in bowel habits.
- Additionally, a large colon polyp can obstruct the bowel, resulting to crampy abdominal pain, nausea and vomiting.
- Bleeding from polyps can occur slowly over time with no visible blood on the patient’s stool. Chronic bleeding robs the body of iron required to produce haemoglobin, which allows red blood cells to carry oxygen to the body. These micro bleeds can slowly make the patient anaemic with all the signs and symptoms related to that.
Tests
Faecal occult blood testing (FOBT), as its name implies, aims to detect subtle blood loss in the gastrointestinal tract, anywhere from the mouth to the colon. Positive tests ("positive stool") may result from either upper gastrointestinal bleeding or lower gastrointestinal bleeding and warrant further investigation for peptic ulcers or a malignancy (such as colorectal cancer or gastric cancer). The FOBT is only used by clinicians as a screening tool for possible colonic polyps or tumours. When it is positive, a colonoscopy is performed.
Diagnosis
Colorectal polyps can be detected using a faecal occult blood test, flexible sigmoidoscopy, colonoscopy, virtual colonoscopy, digital rectal examination or barium enema.
Malignant potential is associated with:
- Degree of dysplasia.
- Type of polyp (e.g. villous adenoma):
- Tubular Adenoma: 5% risk of cancer.
- Tubulovillous adenoma: 20% risk of cancer.
- Villous adenoma: 40% risk of cancer.
- Size of polyp:
- <1 cm =<1% risk of cancer.
- 1-2 cm=10% risk of cancer.
- >2 cm=50% risk of cancer.
Related Information
Normally an adenoma which is greater than 0.5 cm is to be treated.