Indications
Bellow are some common reasons to remove the spleen:
Auto-immune thrombocytopenia purpura (ITP)
This is the most common reason. In this disease, a patient’s platelet count is low because the body makes antibodies to the platelets to destroy them in the spleen. As a result, the patient remaining platelets are not enough to clot the blood and the patient will be at risk of bleeding. The first line of treatment is medical therapy. Splenectomy is only indicated after failing the medical treatment.
Hemolytic anemia
Here, the body makes antibodies against red blood cells. Consequently, they will be destroyed in the spleen. The patient is usually in need of repeated blood transfusion hence the idea of splenectomy to reduce this need.
Hereditary (genetic) conditions
Genetic disorders like spherocytosis, sickle cell disease and thalassemia all result in an abnormally shaped red blood cell. These cells are usually picked up and destroyed by the spleen. Removing the spleen in those patients might make their symptoms better.
Malignancy
Less frequently, patients with lymphoma or leukemia need the spleen removed as it becomes large and remove more platelets. Therefore, splenectomy treat the tumour itself and may improve the blood constituents’ level.
Other reasons
Splenic infarct, aneurysms or splenic abscess
Am I a Candidate for Laparoscopic Spleen Removal?
Yes, if your surgeon is experienced in it and provided the spleen is not massively enlarged.
Diagnosis
- Complete blood count (CBC).
- Bone morrow test is required sometimes.
- CT, Ultrasound, MRI or nuclear scan to complete the diagnosis.
Advantages of Laparoscopic Splenectomy
- Less postoperative pain.
- Shorter hospital stays.
- Quicker return to normal activities.
- Better cosmetic results.
- Fewer incisional hernias.
Preoperative Instructions
- Preoperative immunization against common bacterial infection, 2 weeks before the operation.
- Withhold all anti-platelets and anti-coagulants.
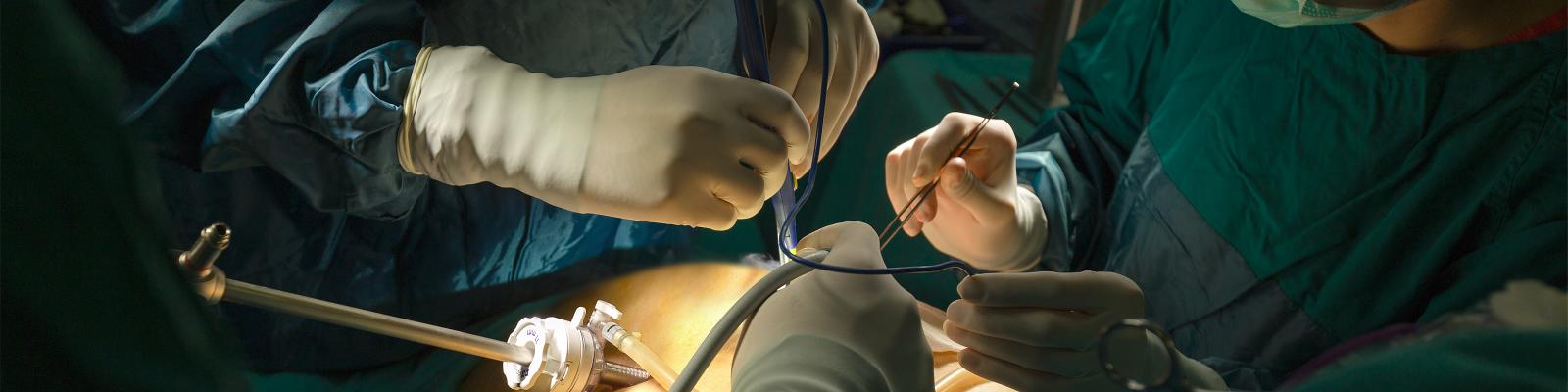
Procedure
- The operation is done under general anaesthesia.
- Laparoscopic instruments are inserted.
- Care is exercised to detect any accessory spleens (10-15%).
- The spleen is mobilised off its attachment and removed completely taking significant care not to injure the pancreatic tail.
Expected Outcomes
- Recovery is usually reasonably fast.
- Few days of hospital stay until diet is tolerated and pain is under control.
Postoperative Instructions
- Antibiotic prophylaxis and infectious disease review.
- Similar to other laparoscopic procedure, diet is normal, full duties can be done after the end of the first post-operative month.
Risks and Complications
- Infective complications (rarely with overwhelming infections)
- Internal bleeding.
- Pancreatitis and pancreatic leak.
When to Call Your Doctor
Be sure to call your physician or surgeon if you develop any of the following:
- Persistent fever with or without signs of wound infection.
- Bleeding.
- Severe abdominal pain.