Introduction
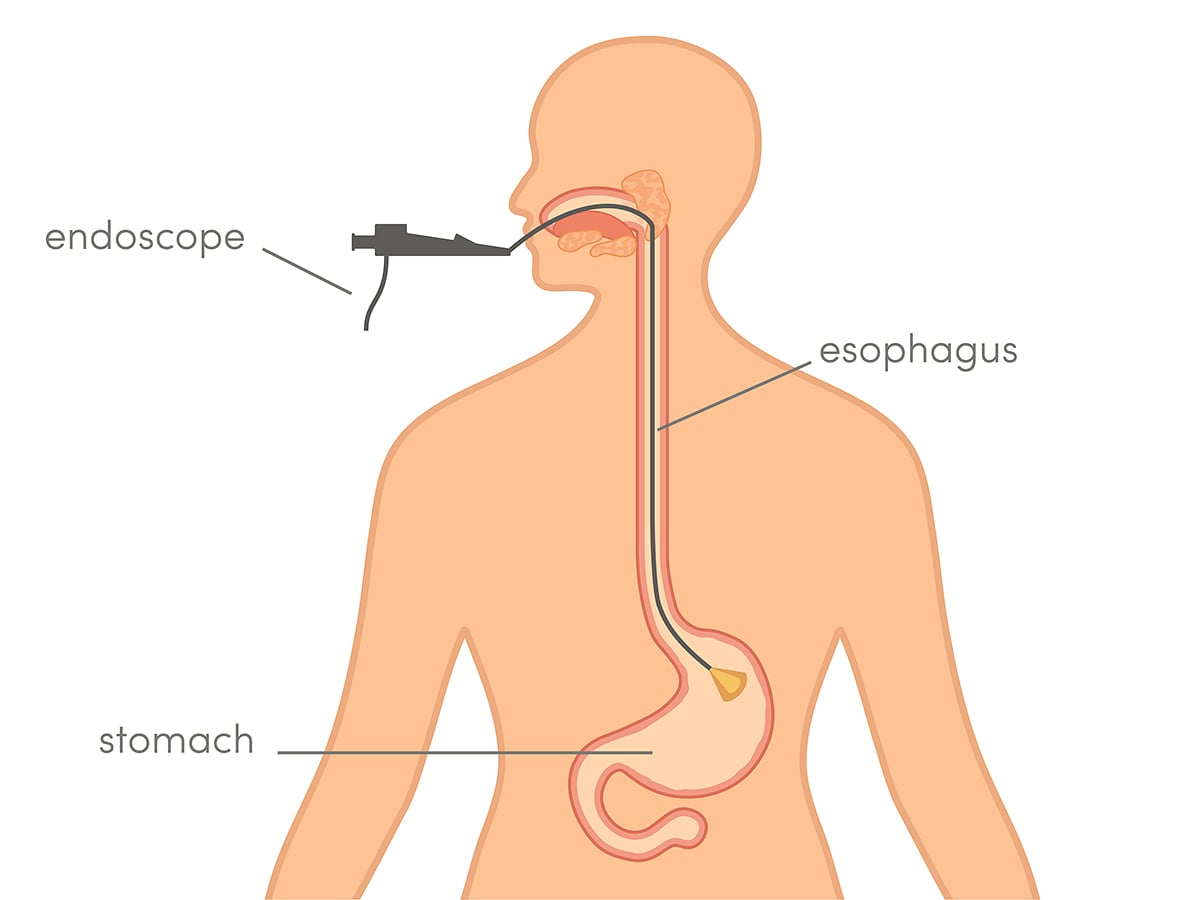
A gastroscopy involves passing the endoscope through the mouth to inspect the entire upper intestinal tract (pharynx, oesophagus, stomach and upper portion of the duodenum) for polyps, ulcers, inflammations, hiatus hernias or reflux disease, tumours and to remove foreign bodies.
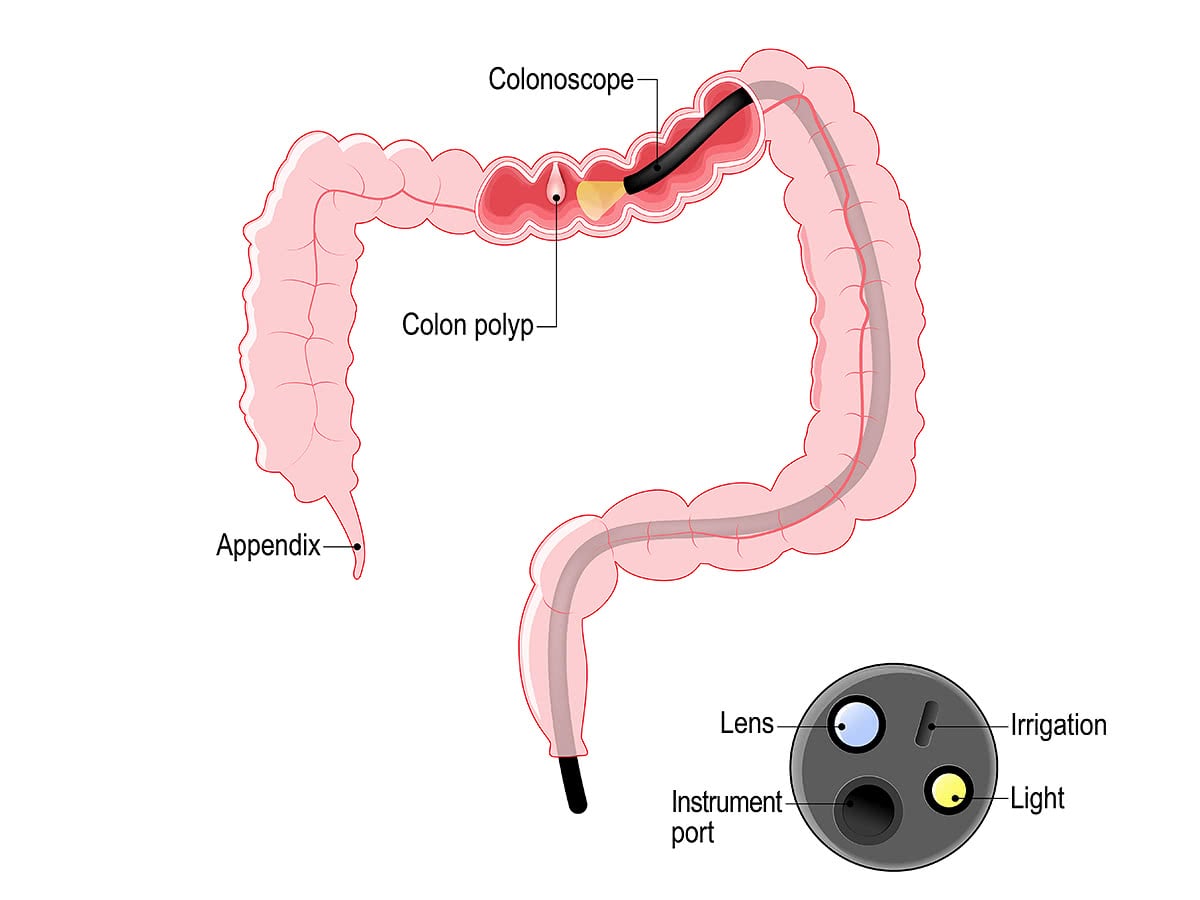
A colonoscopy can remove polyps as small as one millimetre or less. The removed polyps then are sent to the pathology to determine if they are precancerous or not. A polyp to turn into a cancer might take up to 8 years.
Colonoscopy is similar to sigmoidoscopy—the difference is related to which parts of the colon each can examine. A colonoscopy examines the whole colon (1.5 m). A sigmoidoscopy, on the other hand, examines only the distal portion of the colon which may be enough as a cancer surveillance.
CT Colonography is as a totally non-invasive medical test, although it is not standard and still under investigation regarding its diagnostic abilities. CT colonography cannot detect small lesions and it is considered not therapeutic. In other words, we use the test to detect lesions or polyps. If they are detected, a formal colonoscopy should be carried on.
Gastroscopy
Colonoscopy
Indications
Please refer to the section on colonic polyps.
Essential medication information
- Stop IRON TABLETS 10 days before procedure.
- Patients taking medication for HEART OR HIGH BLOOD PRESSURE should take your morning medication with a sip of water at 6am on the day of the surgery unless otherwise instructed.
- Diabetic patients on INSULIN – Do NOT take your morning dose on the day of surgery. Please bring the medication with you to the hospital.
- Diabetic patient on DIABETIC TABLETS - Do NOT take your morning dose on the day of your colonoscopy.
- Do NOT take Non-Steroidal Arthritis medications for 7-10 days as instructed by your doctor (e.g. Voltaren, Nurofen, Advil, Celebrex, Mobic, Naprosyn). If unsure, check with your local pharmacist or your doctor.
- Do NOT take FISH OIL seven days before your procedure.
- DO take your ASPIRIN (e.g. Astrix, Cardiprin, Cartia, Disprin, Solprin, Aspro, Aspro Clear, Bayer Asprin).
- Do NOT take CLOPIDOGREL (Iscover or Plavix) for 7-10 days prior to your colonoscopy as instructed by your doctor.
- Please consult your doctor if you are taking:
- WARFARIN (Coumadin, Marevan).
- RIVAROXABAN (Xarelto), DABIGATRAN (Pradaxa) or APIXABAN (Eliquis).
- PRASUGREL (Effient), TICAGRELOR (Brininta), or DIPYRIDAMOLE (Persantin or Asasantin).
You will be advised as to what action to take by your doctor at least 1 week prior to your surgery date.
Preoperative Bowel preparation Instructions
Two days before your procedure
These items are allowed:
- Boiled or poached eggs.
- Cottage cheese.
- White bread.
- Low fat plain yoghurt.
- Steamed white fish.
- Boiled chicken.
- Well-cooked, peeled pumpkin and potato.
- Clear jelly.
- Skim milk.
- Drink plenty of approved clear fluids.
These items are NOT allowed:
- Brown bread.
- Red meat.
- Cereals.
- Vegetables.
- Anything with seeds in it.
- Nuts.
One day before your procedure
Drink only Clear Fluids – from the moment you wake up.
Clear Fluids – this means fluids that are transparent, or you can see through.
Examples of clear fluids allowed are:
- Water.
- Clear Broth / Soup.
- Apple Juice.
- Grape Juice.
- Black Tea or Black Coffee (NO MILK).
- Jelly (YELLOW OR CLEAR ONLY).
- Cordials (YELLOW OR CLEAR ONLY).
These items are NOT allowed:
- Milk, Cream, Milkshakes.
- Tomato or Orange Juice.
- Soup with vegetables, meat or noodles.
- Solid food of any type (yoghurt and pureed foods are also NOT allowed).
- Chewing gum.
Do NOT eat solid foods – from the moment you wake up.
Instructions for your bowel preparation
These instructions are to assist you in preparing for your surgery and are to commence the day before your surgery. It is extremely important to follow the preparation listed below to enable the doctor to proceed with your surgery. Your colon must be clear of any faecal matter for your surgery to commence. Inadequate preparation may result in the need to reschedule your surgery.
NOTE: Start your Bowel Preparation the day before your surgery as instructed unless you are expecting to be admitted to the hospital the day prior to your surgery. If you are being admitted please phone Wollongong Private Hospital Admissions Office on 02 4286 1000 before commencing your Bowel Preparation.
Procedure and Postoperative Instructions
- It is usually a day case.
- It is usually done under light sedation, The procedure last 20 to 30 minutes.
- The patient then stays in recovery ward for up to 2 hours before he or she is ready to be taken home by relatives.
- At home, normal diet is allowed with Panadol if there is any discomfort.
- Return to activities and work is usually allowed the day after the procedure unless otherwise specified.
- The patient is advised to contact the treating team or present to the emergency of there is severe pain or vomiting or more importantly bleeding or fainting.
- The patient is instructed to have a post procedure review with his surgeon over a few weeks to discuss results.
Risks
The complications are all uncommon:
- Post-procedure pain.
- Distention and discomfort.
- Bleeding and perforation – rare but serious and may require another endoscopy or a surgical operation.