Introduction
Why perform surgery for morbid obesity?
Morbid obesity surgery is not cosmetic surgery. All doctors recognise that once a patient’s weight exceeds a certain range, they are more likely to suffer from a wide range of illnesses such as diabetes, sleep apnoea, asthma, hypertension, arthritis, varicose veins and skin problems. Their chances of dying at a premature age are also greatly increased. Their employment prospects, mobility and social acceptance also suffer. Depression is much more common in the morbidly obese.
The main aim of this surgery is to bring your weight down to a safer range where most of these associated conditions are reduced in severity and many completely reversed. Along the way most people find an improvement in their mobility, body image, self-esteem and enjoyment of life.
Indications
- Body mass index (BMI) ≥40 kg/m2 with or without any associated comorbidities.
- BMI between 35 and 40 kg/m2 with at least one serious weight-related comorbidity, including but not limited to diabetes, obstructive sleep apnoea, hypertension, and coronary artery disease.
In addition, LSG may also be indicated for patients with:
- BMI between 30 and 35 kg/m2 with uncontrollable type 2 diabetes or metabolic syndrome.
Besides being a primary bariatric operation, Laparoscopic Sleeve Gastrectomy (LSG) has also been used as a bridging procedure in super morbid obese patients (BMI of 50 kg/m2 and above) before biliopancreatic diversion with duodenal switch. Additionally, LSG is also a good revision procedure for patients who fail laparoscopic adjustable gastric banding.
LSG is safe for patients with diabetes, metabolic syndrome, and inflammatory bowel disease. Although some bariatric surgeons disagree, the majority of the experts consider LSG an effective treatment for type 2 diabetes. LSG can also be offered to high-risk patients such as those with Child's A or B liver cirrhosis and those awaiting kidney or liver transplant (with the goal of improving future graft function or heart transplant).
Preoperative Instructions
Prior to any bariatric surgery, patients need to undergo psychologic, medical, and anaesthetic risk assessment.
Prior to LSG, patients with upper gastrointestinal tract symptoms (e.g., acid reflux, dysphagia) can be evaluated, at the surgeon's discretion, with an upper gastrointestinal contrast series (UGI) and/or an oesophagogastroduodenoscopy (EGD) to exclude ulcers, polyps, masses, or dysplastic changes and to identify any anatomical abnormalities such as a hiatal hernia.
Such patients may also undergo oesophageal pH testing and manometry to assess the severity of any existing gastro-oesophageal reflux disease (GERD) and exclude oesophageal motility disorders. Although oesophageal motility disorders such as achalasia are not considered contraindications to LSG, they could potentially be addressed before or at the same time of LSG.
Procedure
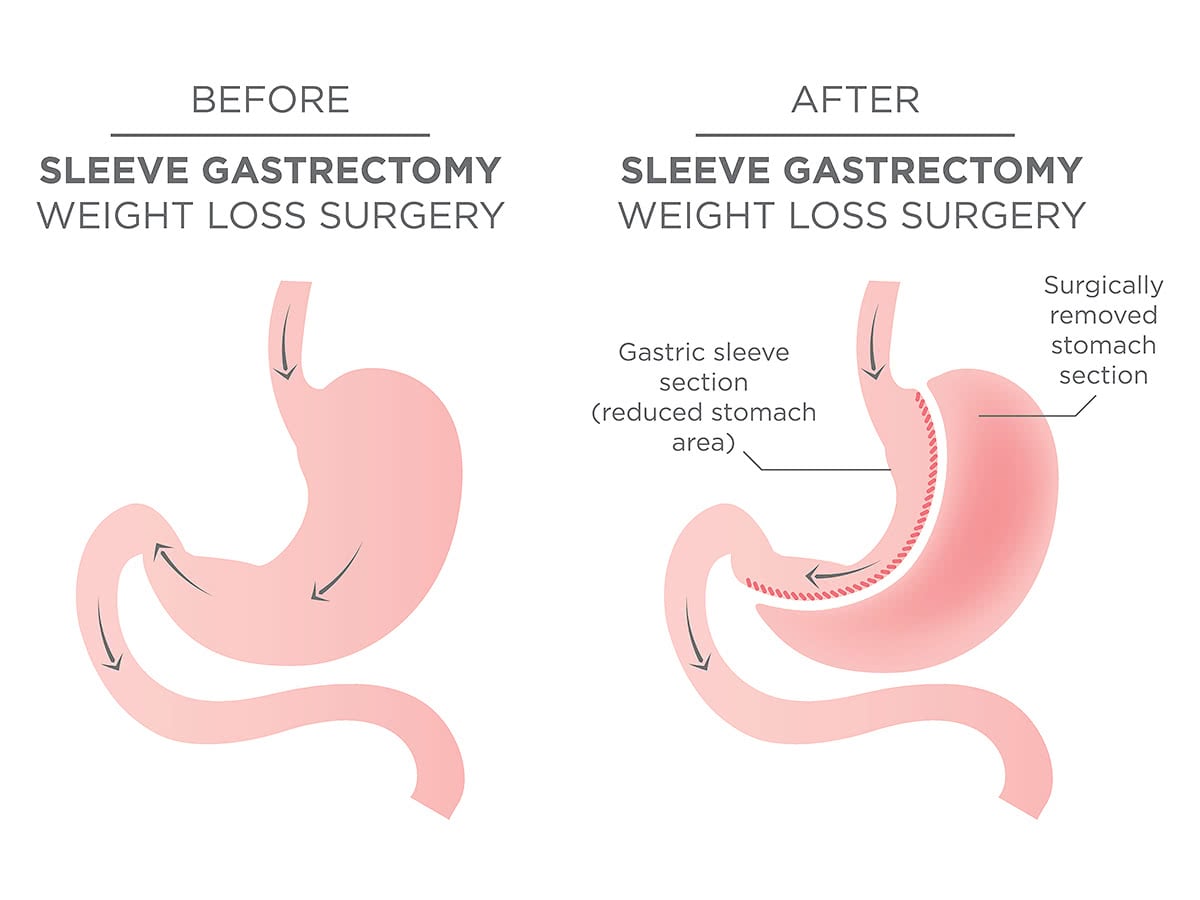
The aim of the procedure is to restrict the stomach. This can be achieved by cutting some 70-75% of the stomach longitudinally to make it looks like a sleeve. As a result, the patient will have a smaller reservoir. This can be achieved by using a cutting-stapling device.
The operation works by making the stomach smaller, means the patient will eat less and still feel full. Moreover, the operation removes the area that releases the hunger hormone which means the patient will feel less hungry.
Sleeve gastrectomy does not have any mal-absorption component to it which makes it different to Gastric Bypass operation in which part of the small intestine is bypassed to reduce the nutrient absorption thereby reducing the patient weight.
Postoperative Instructions
Despite considerable national variation in clinical pathways used by bariatric centres, most patients are admitted for overnight observation or more after LSG, especially if they have a history of obstructive sleep apnoea. Postoperative nausea is the most common complaint and should be treated with scheduled doses of intravenous antiemetics.
Risks and Complications
- Sleeve gastrectomy is relatively new and has not been evaluated as much gastric banding or gastric bypass.
- Sleeve gastrectomy is irreversible.
- Complication risks are slightly higher than with Lap-band mainly bleeding and staple line leak.